Interesting Points
During the course of my investigation I have uncovered some interesting things:
Most of the medical opinions obtained thus far were based on the gastrograffin being aspirated into my lung wheras it was actually placed into my lung - a huge difference. To read the comments from medical experts so far please click on "medical opinions" link.
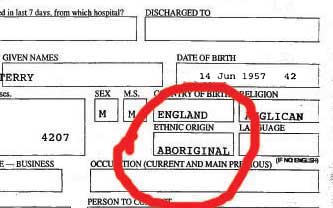
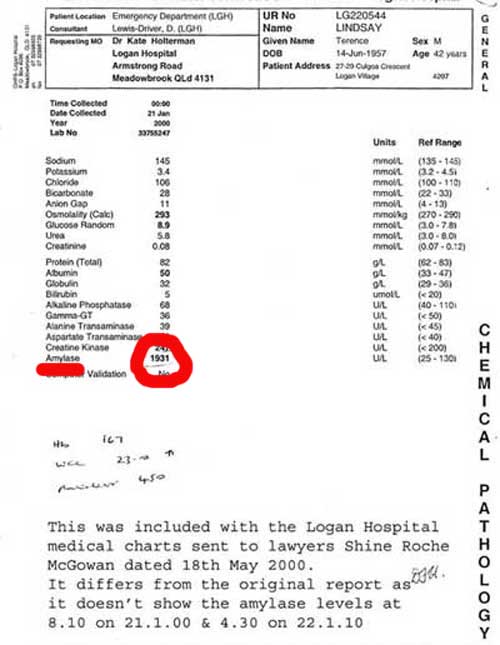
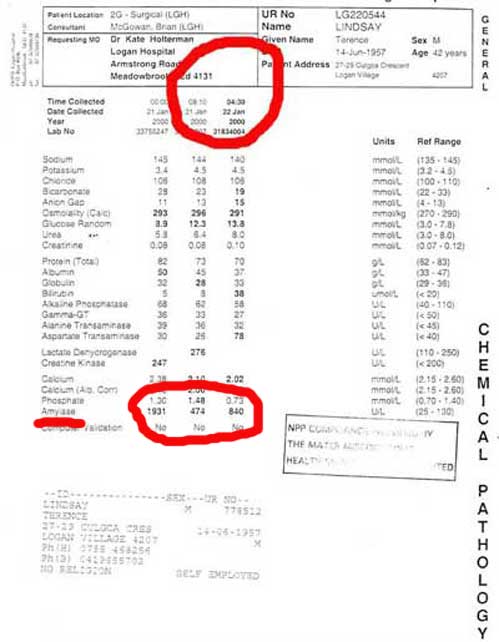
When I first commenced legal action it was with Shine Roche McGowan lawyers. This was organised by my brother in law. He had a knee jerk reaction as soon as he heard that a mistake had been made and commenced litigation. All this did was alienate everybody. The hospital doctors closed ranks, records were hard to find and nobody wanted to give an opinion. When the lawyers came in to see me I had just come out of intensive care. I had no idea what they were talking about. In hindsight I wish my family would have waited until I recovered so I could have carefully investigated my options before contacting lawyers. The only thing that was achieved was securing my statute of limitations. Shine Roche McGowen put my case in the too hard basket so I contacted The Health Rights Commission, which are part of Qld Health. They obtained a medical opinion from a specialist in intensive care. It was agreed that all of my records for both The Logan Hospital & The Mater Hospital along with records from my local GP would be sent to this specialist for an expert opinion. Unfortunately, as this doctor was going away on holidays and as the Health Rights Commision did not want to miss the opportunity to obtain a report from him, they just sent a two page summary outlining my medical history. I thought this totally inadequate, and subsequently most of the questions were answered based on his experience of acute pancreatitis alone and not from my medical records. One question in particular where I asked the doctor "what affect would 400mls of 2% gastrograffin have if aspirated into the left lung of a healthy male". The reply was " We could not deny that a severe problem could occur but could not find any literature to support this".The Health Rights Commission agreed to send all of my records to the specialist for a second opinion. He answered the questions on pancreatitis and multiple organ failure quite clearly but could find anything on gastrograffin aspiration or how this would affect pre-existing acute pancreatitis. I asked the question " what would the effect be of 400mls of 3% gastrograffin aspirated (actually placed) into my left lung". The answer was "I have researched the medical archives from 1966 to 2002 and cannot find any incidents of this occuring but in Mr Lindsay's case he already had a severe case of acute pancreatitis and I feel this contributed to all of his problems".
I researched "gastrograffin in the lungs" in Google and I was inundated with information of how dangerous it is. It appears that it is extremely dangerous when put into the lungs. The solution is iodine based and hypersmolar absorbing all of the moisture from my organs. I even contacted a surgeon in Scotland who initally didn't believe that it was gastrograffin that I had instilled into my lung as he said that I would not have survived. "It would have caused massive pulmonary oedema and your demise". He advised me to check that it was actually gastrograffin that was instilled. I confirmed that it was and sent him a copy of my medical reports. He said that I was lucky to have survived!
I have established that gastrograffin at 3% solution would be hypertonic and therefore cause severe hypoxia and pulmonary oedema. This starved my body of oxygen. It is quite obvious that this would have affected a pre-existing condition such as acute pancreatitis. The problem is proving it in court! My lawyers have advised me that there must be "causation". In other words, what the caregiver did or neglected to do , actually caused objective and measurable damages to the care receiver. "Measurable" being the key word. I have found it near impossible to find an expert to quantify how much of my injures were a result of the mistake and how much by my pre-existing pancreatitis. I did obtain a medical report from a physician and when asked to quantify how much of my overall condition was attributable to their mistake he commented " I think that 2% of the patients overall condition was attributable to the gastrograffin aspiration (placement)". "This is purely my opinion and I have no way to substantiate it". Surely this opinion can't be taken seriously! It should be backed up with medical fact.
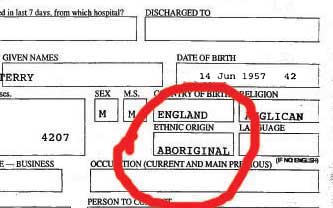
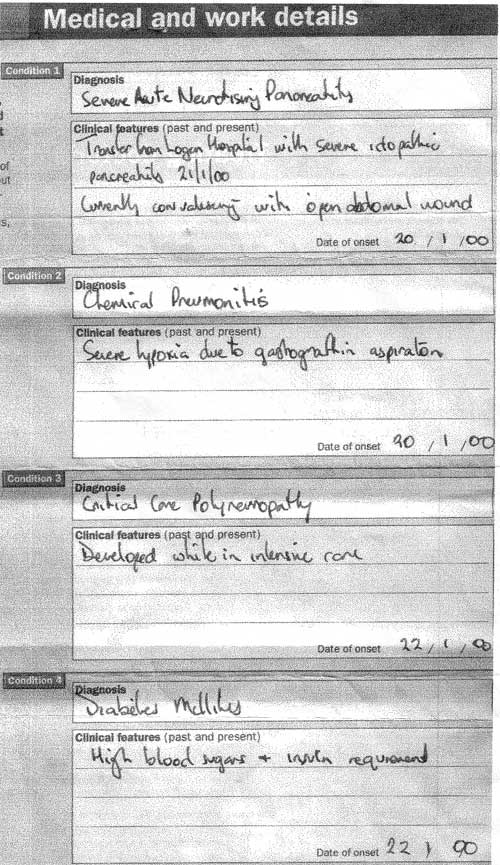
There has been a lot of discussion on whether the gastrograffin placement into my lungs would have caused hypoxia which in turn contributed to the severity of my pre-existing acute pancreatitis. Below is a copy of my medical & work details report which was completed by the surgeon that saved my life. It clearly states under condition 2 " Chemical pneumonitis - servere hypoxia due to gastrograffin aspiration".
Why did the hospital use gastrograffin for the examination of my gut when I had a pre-existing pancreatic condition? Gastrograffin placement into the lung causes severe hypoxia and pulmonary oedema. They should have used barium which is better tolerated if accidently aspirated or placed into the lung. I feel that the hospital deviated from the accepted standards of care in using gastrograffin contrast. Gastrograffin aspiration can severely affect a patient's respiratory function . This would have been disastrous for a patient such as myself with pancreatitis which was already showing signs of producing respiratory problems.
After the gastrograffin incident why was I not put into intensive care? If no beds were available at The Logan Hospital I should have been transferred immediately to another hospital. Because of the elapsed time between when the incident happened and when I was transferred to The Mater Hospital my condition worsened. The Logan Hospital was negligent in failing to transfer me to ICU immediately after the incident for continuous oximetry and cardiac monitoring.
Below is a medical malpractice case where the improper use of gastrograffin caused significant pulmonary difficulties increasing the risk of respiratory failure and deprivation of oxygen. From my understanding this patient had 50mls of gastrograffin aspirated into the lung wheras I had 400mls placed into my lung. Article printed courtsey of James P McCarthy, Boston MA.
|
